| Overview : This
lecture builds on the material we explored in a previous lecture on schizophrenia.
The main purpose of the lecture is to show you how behavioural
techniques can be used to discover more effective drug treatments for
schizophrenia. The lecture begins with a brief rationale for the use of
drugs to treat schizophrenia, before moving on to consider side effects
associated with the use of the largest group of antipsychotic drugs,
so-called classic antipsychotics. The location and
roles of the nigrostriatal and mesolimbic dopamine system in EPS and
symptom control are described. The strengths and weaknesses of the Discriminated
Avoidance Inhibition Model as a screening technique are
explored before reviewing the Amphetamine-Induced Stereotyped
Behaviour Model . The similarities and differences between
classic and atypical antipsychotics are presented as a rationale for
introducing a new screening technique - the Amphetamine-Induced
Stereotyped Locomotion Model . In this model hyperactivity
and stereotypy of amphetamine
treated rats can be measured separately. Finally the effects of an
atypical drug are examined in this new screening technique. |
Evidence for
Biological Basis of Schizophrenia
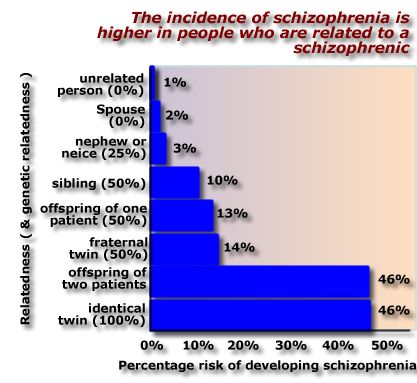 |
Three lines of evidence suggest that schizophrenia has a biological basis:
|
Diagnosis
and Treatment of Schizophrenia
|
Diagnosing schizophrenia should be carried out by a psychiatrist using criteria set out in a diagnostic manual (e.g. DSM-III-R). In brief, schizophrenics typically suffer from delusions (e.g. paranoia), hallucinations (auditory and visual), disordered thought, inappropriate emotional behaviour, social withdrawal, and apathy. Lickey and Gordon (1991) provide a clear and detailed description of the difficulties and uncertainties involved in diagnosing schizophrenia.
Antipsychotic drugs are also known by the older terms:
This diagram shows the percentage of patients treated successfully with each of four different treatment methods. Successful
treatment was defined as release
from the hospital within one year. Redrawn from data in May (1968). |
Reduced Relapse Rates by Combining Psychological & Drug Therapies
| Although
antipsychotic drugs alleviate the symptoms of schizophrenia, about 90%
of patients eventually relapse (the symptoms
return) if they stop taking medication.
Furthermore, about 40% of patients relapse - even if they continue to take an antipsychotic drug.
Notice the dramatic reduction in relapse by combining drug with social skills training and family therapy. Figure drawn from data in Hogarty et al (1986). |

Figure drawn from data in Hogarty et al (1977).
|
Side
Effects of Classic Antipsychotics
If, combining drug and psychological therapies produces low relapse rates you might think that the problem of schizophrenia has been solved . Unfortunately most antipsychotic drugs produce side effects as well as controlling the disease. The most commonly used antipsychotic drugs - typical or classic antipsychotics - cause very unpleasant side effects.
Classic
antipsychotics produce a constellation of disordered
movements called the extrapyramidal syndrome (EPS) .
EPS is thought to be caused by effects of classic antipsychotics on the
extrapyramidal system of the brain.
These observations suggest that the EPS may be the result of classic antipsychotic drugs blocking receptors in the nigrostriatal DA system. |
Extrapyramidal Side
Effects
Source: Diaz (1977). |
There are a number of collections of nerves in the brain that release dopamine.
Two systems have been implicated in the behavioural effects of antipsychotic drugs.
|
The
Need for Novel Antipsychotic Drugs
|
When antipsychotic drugs were first used, some psychiatrists increased the dose of the drug until extrapyramidal side effects (EPS) appeared. They believed that the appearance of side effects indicated that sufficient drug had been given to affect the patient's schizophrenic symptoms (figure redrawn from data in Marsden et al, 1986, table 12.2). However antipsychotic drugs
Consequently there is no evidence to support the view that the appearance of EPS is a sign of clinical effectiveness. This diagram was constructed from data in Marsden et al, (1986, Table 12.2) and shows that the risk of developing extrapyramidal side effects is not the same for all types of antipsychotic drugs. i have included the table of raw data to show how I calculated the statistic 'Cumulative percentage of patients with EPS'. This data will be used later in this lecture when we discuss the link between EPS and discriminated avoidance behaviour. |
| Percentage of patients exhibiting side effects under placebo and three antipsychotic drugs | |||||
 |
Extrapyramidal side effect (EPS) | Placebo | Thioridazine | Chlorpromazine | Fluphenazine |
| Muscle rigidity | 8.1 | 4.4 | 12.5 | 24.2 | |
| Facial rigidity | 5.4 | 8.8 | 12.5 | 14.3 | |
| Tremor of hands, arms and face | 5.4 | 13.2 | 5.7 | 12.1 | |
| Loss of associated movements | 2.7 | 0 | 3.4 | 19.8 | |
| Akathisia | 4.1 | 3.3 | 5.7 | 12.1 | |
| Increased salivation | 0 | 3.3 | 5.7 | 8.8 | |
| Dystonia | 0 | 1.1 | 4.5 | 6.6 | |
| Oculogyric crisis | 0 | 0 | 1.1 | 0 | |
| Cumulative percentage with EPS | 25.7% | 34.1% | 51.1% | 97.9% | |
There is clearly a need for new antipsychotic drugs that possess the beneficial effects of classical antipsychotics in treating schizophrenia, but lack the potential to cause extrapyramidal side effects. There is good reason to believe that that it will be possible to develop new drugs with this profile of effects. For example, in an earlier part of your course you learned about atypical antipsychotic drugs. Atypical antipsychotics (e.g. sulpiride and clozapine) are as effective as older classic antipsychotics in controlling the symptoms of schizophrenia, but do not cause EPS.
Unfortunately these drugs have other side effects (e.g. clozapine causes agranulocytosis ), and therefore the search continues for an effective treatment for schizophrenia.
The rest of this lecture is concerned with behavioural screening tests that have been employed to detect novel antipsychotic drugs.
Discriminated Avoidance Inhibition Model
 Carlton
(1983) describes an important
behavioural technique that could be used to detect antipsychotic drugs.
Rats are first
trained to avoid or escape shock on a discriminated
avoidance schedule.
Carlton
(1983) describes an important
behavioural technique that could be used to detect antipsychotic drugs.
Rats are first
trained to avoid or escape shock on a discriminated
avoidance schedule.
In this situation the animal:
When rats - that have successfully learnt to avoid shock - are injected with antipsychotic drugs they:
The diagram (redrawn from Cook & Sepinwall, 1975) shows that chlorpromazine disrupts avoidance behaviour, but has no effect on escape behaviour. Avoidance disruption is dose dependant. Higher doses cause more disruption. But even at the highest dose, escape behaviour remains unaffected. I have magnified the bottom part of the graph to emphasize this important difference between the effect of the antipsychotic on avoidance and escape behaviours.
These findings
are encouraging. The next step is
to investigate a large number of antipsychotic drugs to confirm that
they all exert this differential
effect on avoidance-escape behaviours, and examine their relative
potencies.
 In
common with all types of
drugs, antipsychotics differ in their clinical potencies. Some drugs
must be administered
in large doses to control schizophrenic symptoms. Others are more
potent, the patient can
be given a smaller dose to produce the desired clinical effect. Drugs
also differ in their
ability to affect animal behaviour. ED50 avoidance is
the dose of the drug that -
when injected - disrupts avoidance behaviour by 50%. The ED50 value is
calculated from the
drugs dose response curve. Therefore it is an Estimated
Dose.
In
common with all types of
drugs, antipsychotics differ in their clinical potencies. Some drugs
must be administered
in large doses to control schizophrenic symptoms. Others are more
potent, the patient can
be given a smaller dose to produce the desired clinical effect. Drugs
also differ in their
ability to affect animal behaviour. ED50 avoidance is
the dose of the drug that -
when injected - disrupts avoidance behaviour by 50%. The ED50 value is
calculated from the
drugs dose response curve. Therefore it is an Estimated
Dose.
These results confirm the impression that antipsychotics disrupt avoidance behaviour. Furthermore, there is high correlation between the amount of drug needed to disrupt avoidance in the rat, and the dose used to treat schizophrenia. Nevertheless, there is an important ' outlier ' value.
This table
includes the raw data I used to
construct the figure. I have included this information because there is
considerable
clustering of drugs with ED50 values <1 mg/kg. Source: Carlton (
op cit ). In addition,
the table suggests that there may be a correlation between a drug's
effect on avoidance
behaviour in rats and tendency to produce EPS in humans
| Drug | ED50-Avoidance | Median daily dose | Cumulative percentage with EPS |
| promazine | 24.7 | 2085 | |
| clozapine | 7.2 | 1538 | |
| mesoridazine | 6.5 | 412 | |
| thioridazine | 5 | 788 | 34.1% |
| molindone | 2.5 | 122 | |
| chlorproyhixene | 1.9 | 330 | |
| thiothixene | 1.9 | 38 | |
| chlorpromazine | 1.8 | 750 | 51.1% |
| triflupromazine | 0.87 | 285 | |
| prochlorperazine | 0.44 | 105 | |
| fluphenazine | 0.37 | 8 | 97.9% |
| trifluoperazine | 0.3 | 22 | |
| perphenazine | 0.24 | 68 | |
| pimozide | 0.23 | 8 | |
| haloperidol | 0.16 | 8 |
These results suggest that:
 |
In essence I am suggesting that the strong correlation between a drugs potency in the animal test and the clinic may be linked to the tendency for some drugs to affect the extrapyramidal motor system. This is a plausible connection because any drug which interfered with an animl's motor function would be expected to disrupt performance on the discriminated avoidance task.
| Point to ponder: Could the differential effect of classic antipsychotic drugs on avoidance and escape behaviours be explained in terms of drug effects on the extrapyramidal system? |
Does
Discriminated Avoidance Inhibition Predict EPS?
We now know that antipsychotic drugs produce two effects in patients:
We need to be certain that a screening test for improved antipsychotic drugs predicts clinical improvement. Clearly there is little value in a screening technique that is based on a drugs ability to produce unwanted side effects in patients, (unless that is the primary purpose of the test). There is further evidence that disruption of discriminated avoidance responding is an indication that the drug will produce EPS in patients. For example, consider the following profile of action shown by drugs that effect the cholinergic system.
| Effect on cholinergic system | Effect on EPS in humans | Effect on discriminated avoidance in rats |
| Interfere with the cholinergic system (anticholinergic ) | Reduce EPS | Reduce effect of antipsychotics |
| Facilitate the cholinergic system ( cholinomimetic ) | Increase EPS | Disrupt avoidance behaviour |
The effects of cholinergic drugs on discriminated avoidance behaviour suggests that
These findings are consistent with the notion that neuroleptic disruption of avoidance predicts EPS potential, rather than antipsychotic potential.
Amphetamine-Induced
Stereotyped Behaviour Model
We have seen that the Discriminated Avoidance Inhibition Model may have limited usefulness in detecting the antipsychotic potential of new drugs. But there are other ways of discovering new safer drugs that could be used to treat schizophrenia.
A well established screening test for novel antipsychotic drugs involves examining their ability to antagonize the effects of amphetamine on animal behaviours. We have studied this model in detail in a previous lecture . Here is a brief overview.
Injecting animals,
usually rats, with amphetamine produces:
A
behaviour is said to be stereotyped when it is is
repeated in an apparently meaningless fashion.
|
|
 |
Amphetamine-induced increases in locomotion are particularly marked at relatively low doses (less than 4 mg/kg) of the drug.
As we saw in an earlier lecture , classic antipsychotic drugs (e.g. pimozide)
However, atypical antipsychotics (e.g. clozapine)
Importantly both atypical and classic antipsychotics antagonize amphetamine-induced hyperactivity.
Amphetamine-Induced
Stereotyped Locomotion
It is now time to pull together a number of things discussed in this lecture to see if we can construct a new model of antipsychotic potential
Some relevant
observations from previous research:
Here is a table setting out these findings |
|||||||||||||||||||||
|
This
analysis suggests that:
We began a series of experiments to test this hypothesis see: Kenyon, Moore & Hampson, ( Current Psychology: Research & Reviews , 11, 241-253, 1992) |
||||||||||||||||||||
| Point to ponder
What would be the advantages of having an animal model of schizophrenia that distinguished between classic and atypical antipsychotic drugs? |
Measuring
Amphetamine-Induced Stereotyped Locomotion
In order to classify a response as stereotyped it should be exhibited in a repetitive and invariant fashion. Several years ago Schiorring (1979) pointed out that locomotion under amphetamine exhibits stereotyped properties.
This means that we can use one behaviour (locomotion) to study the effects of antipsychotic drugs on both amphetamine-induced hyperactivity and stereotyped behaviour.
 An
open-field is a
large box with lines drawn on the floor that divide the floor into four
quadrants. The rat
is put on the floor, and its movement between quadrants is recorded.
Mueller et al.(1989)
introduced a way to measure stereotyped locomotion
in the open-field test.
An
open-field is a
large box with lines drawn on the floor that divide the floor into four
quadrants. The rat
is put on the floor, and its movement between quadrants is recorded.
Mueller et al.(1989)
introduced a way to measure stereotyped locomotion
in the open-field test.
|
|
Mueller developed a statistic - called gamma - to measured the repetitiveness in locomotion.
The number of repeat and change trips are entered into a formula to calculate the gamma statistic.
Gamma = (Repeat trips)/(Repeat trips + Change trips)
In this example Gamma = (1)/(1+4)=0.20
Computer
Based System for Recording
Locomotion
 The
diagram shows the apparatus Kenyon et al (1992) used to record the
effects of amphetamine
on locomotion. The open-field test apparatus is a simple open topped
box with 1 metre
sides painted black to provide contrast with the white rat.
The
diagram shows the apparatus Kenyon et al (1992) used to record the
effects of amphetamine
on locomotion. The open-field test apparatus is a simple open topped
box with 1 metre
sides painted black to provide contrast with the white rat.
A videocamera is suspended directly over the centre of the open-field. The image from the camera is fed into a digitizer which locates the position of the white rat against the black background of the apparatus. The position of the rat is translated into a stream of X,Y co-ordinates which represent the position of the rat as it moves around the open-field. This data stream is fed into a computer which displays the position of the rat on a screen and stores the X,Y values.
After
the test session the data stream is
analysed and the locomotion of the rat is broken down into distance
moved per minute and
the number of trips of various lengths (1 through 4 see above
for definition of Trip Lengths)
| Point to ponder
What properties of stereotyped locomotion are not measured by this apparatus? |
Distance
Moved Under Amphetamine & Sulpiride
 |
The diagram shows the
mean distance moved by four independent groups of rats:
Results:
|
Increase
in Length 4 Trips Under Amphetamine
| We also found that
amphetamine produced an increase in repetitive (stereotyped?) walking
around the sides of the apparatus. This was reflected by an increase in
the number of Length 4 trips under amphetamine.
The diagram shows the number of complete trips around the perimeter of the apparatus ( Length 4 trips) per 5 min during the 105 min test period. Sulpiride significantly reduced the number of length 4 trips in amphetamine treated rats (compare the behaviour of the Sulpiride+amphetamine group with the Vehicle+amphetamine group).
|
 |
Lack
of Effect of Sulpiride on the Proportion of Length 4 Trips Under
Amphetamine
| Pre-treatment with
sulpiride reduces the amphetamine-induced increase in Length 4 trips.
This might lead you to conclude that sulpiride reduces the stereotyped
locomotion produced by amphetamine but, as we have already seen, rats
injected with sulpiride + amphetamine show less activity than rats
injected with just amphetamine (Vehicle+Amphetamine group). Therefore
the reduction in Length 4 trips might just be the result of the animal
moving around less in the open-field.
This led us to focus on the proportions of Length 4 trips in the Vehicle+Amphetamine and Sulpiride+amphetamine groups. |
|
 |
The diagram shows the
effect of sulpiride pretreatment on the proportion of Length 4 trips
under amphetamine:
Conclusion:
|
Gamma Scores
Under Amphetamine & Sulpiride
Kenyon
et al's (1992) results provoke a series of questions:
The first question is the most important. It gives any scientist greater confidence if their results can be replicated by an independent laboratory. Fritts, Mueller and Morris (19970 have found that sulpiride (25mg/kg) does not reduce amphetamine-induced stereotyped locomotion. They used Mueller's gamma statistic which is a measure of the sameness in the rat's trips around an open-field. This result confirms our impression that sulpiride exerts a differential effect on amphetamine-induced behaviours. Locomotion is reduced, but the stereotyped nature of locomotion under amphetamine is not abolished by atypical antipsychotic drugs. But that still leaves two unanswered questions ... |
 |
Direct comparison of classic and atypical antipsychotic drugs on stereotyped locomtion
| Points to
ponder What would you expect classic antipsychotic drugs to do to the proportion of Length 4 trips? How would you improve this experiment to include the properties of stereotyped locomotion that were not measured in this study? |
Moore & Kenyon
(1994) examined the effects the classic antipsychotic haloperidol, and
two atypical antipsychotics - sulpiride and clozapine for their ability
to antagonize
The results presented below indicate that
|
||||||||||
 |
 |
|||||||||
References
Supplementary Material
|